
Colorectal cancer, or CRC, is a disease of the colon or rectum, which are parts of the digestive system. Unlike most cancers, colorectal cancer is often preventable with screening and highly treatable when detected early. Most cases of colorectal cancer occur in people ages 45 and older, but the disease is increasingly affecting younger people. Each year, about 150,000 Americans are diagnosed with this disease and more than 50,000 die. However, colorectal cancer can be prevented with screening because it's highly treatable when caught early.
In recognition of National Colorectal Cancer Awareness Month, we want to explain what colorectal cancer is, how it starts, how it's treated, and how getting screened can mean the difference between life and death. Summit Medical Group offers colorectal screening options for patients at average or above-average risk. For more information, visit www.summitmedical.com.
About CRC
Colorectal cancer is the second most common cancer in the US among men and women combined. It is estimated that approximately 1 in 24 people will get colorectal cancer in their lifetime. But it is highly treatable when it is discovered early. Even if it spreads into nearby lymph nodes, surgical treatment followed by chemotherapy is very effective. Studies show that with early detection, CRC has a 90% survival rate.
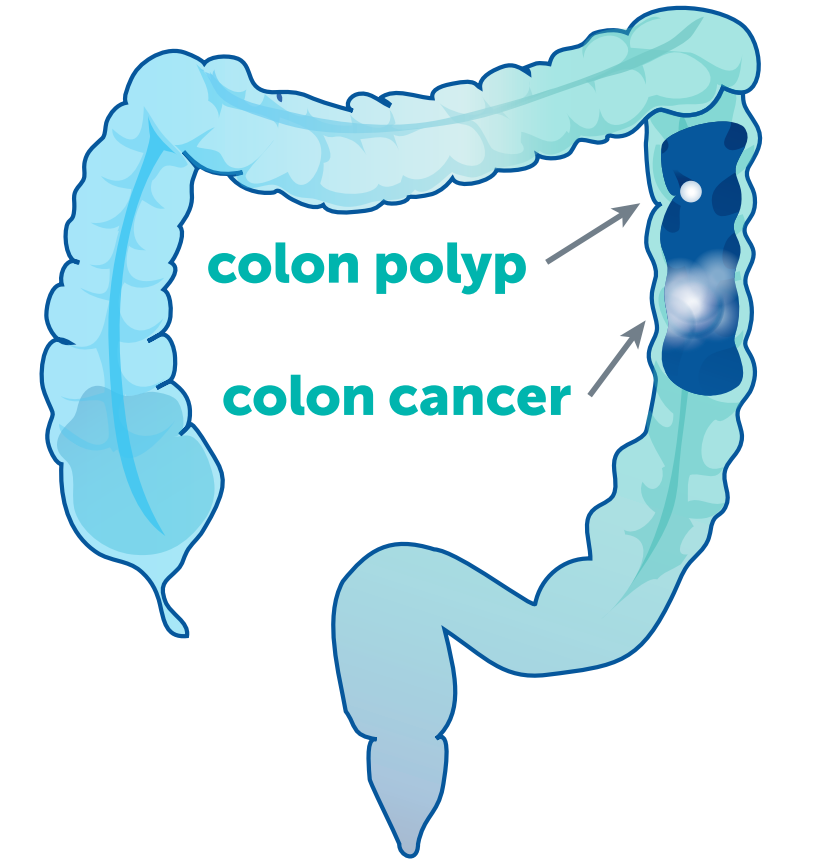
Most colorectal cancers start as an abnormal tissue growth, called a polyp, inside the colon or rectum. With the help of screening tests, doctors can detect polyps, remove them, and prevent them from developing into colorectal cancer. In the most advanced cases — when the cancer has spread to the liver, lungs, or other sites — chemotherapy can often make surgery an option, prolonging and adding quality to life. Research is ongoing to learn more about this disease and provide more hope to people with all stages of colorectal cancer.
Symptoms
Colorectal cancer may not cause symptoms, particularly at first. Someone can have colon cancer or rectal cancer and not know it. That's why every person should get screened starting at age 45. People at higher risk may need to get checked earlier, according to their risk factors. When they occur, symptoms may include:
- Changing bowel habits
- Changing bowel habits may include intermittent or constant diarrhea and/or constipation, a change in the consistency of your stool, or stools that are more narrow than usual
- Unexplained weight loss
- A loss of weight for no known reason should always be investigated. Nausea and/or vomiting are also possible symptoms
- Inflammatory bowel diseases such as Crohn's disease or ulcerative colitis
- A personal or family history of colorectal cancer or colorectal polyps
- A genetic syndrome such as familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (Lynch syndrome)
- Black/African Americans and Ashkenazi Jews are at higher risk
- Persistent abdominal discomfort
- Abdominal discomfort may present as cramps, gas, or pain. You may also feel full, bloated, or like your bowel is not completely empty. Nausea and vomiting can also be a symptoms.
- Rectal bleeding
- Blood in or on your stool is a symptom of rectal cancer and colon cancer. The blood can be bright red, or the stool may be black and tarry or brick red.
- Weakness and/or fatigue
- Weakness and/or fatigue may be a sign of colorectal cancer. Weakness and/or fatigue may be accompanied by anemia or a low red blood cell count.
However, it's important to note that the most common symptom of colorectal cancer is NO symptom at all. This is why regular screenings starting at age 45 are so important! While anyone can develop colorectal cancer, a few conditions can increase risk, which may mean you need to start the screening process earlier. These risk factors include:
Screening Saves Lives
With screening, colorectal cancer is one of the most preventable cancers. Colon cancer and rectal cancer are also highly treatable if caught early. However, 1 out of every 3 eligible adults are not getting screened. As mentioned earlier, Colorectal cancer almost always develops from precancerous polyps (abnormal growths) in the colon or rectum. Screening tests can find precancerous polyps, so that they can be removed before they turn into cancer. Screening tests can also find colorectal cancer early, when treatment works best.
All men and women should be screened for colorectal cancer. Your individual risk factors will determine when you should start getting checked. The following table provides a list of situations and when screening is recommended:
| IF YOU: | THEN YOU SHOULD: |
|---|---|
| Are experiencing symptoms | Talk to your doctor immediately, regardless of your age or family history. |
| Have a family history of colorectal cancer or polyps | Get screened at age 40 or 10 years before the age of the youngest case in your immediate family (mother, father, sister, brother). |
| Are African American | Get screened at age 45. |
| Have a genetic link to colorectal cancer such as Lynch Syndrome, FAP, etc. | Family members who tested positive for a relevant mutation(s) should start colonoscopy screening during their early 20s, or 2 to 5 years younger than the youngest person in the family with a diagnosis, and repeat it every 1-2 years. Family members who have not been tested yet should be screened during their early 20s, or 2 to 5 years younger than the youngest person in the family with a diagnosis. |
| Have a personal history of cancer | Talk to your doctor and get screened before age 45. |
| Have ulcerative colitis, inflammatory bowel disease or Crohn's disease | Talk to your doctor about getting screened before age 45. |
CRC Screening Methods
There are many CRC screening methods available. Because you have options, it's important to discuss them with your healthcare provider. What is most important is empowering yourself to understand these different options so you can advocate not only for yourself, but for those you care about too.
The table below provides the list of CRC screening methods that includes a description, test frequency, as well as the pros and cons of each. Finding the best option(s) that fit your routine, personal preference, and comfort level matter. Your doctor should guide you, but ultimately you can proactively advocate for the option that suits you best.
COLONOSCOPY
| WHAT AND HOW |
|
| FREQUENCY |
|
PROS |
|
| CONS |
|
STOOL DNA
| WHAT AND HOW |
|
| FREQUENCY |
|
PROS |
|
CONS |
|
FECAL IMMUNOCHEMICAL TEST (FIT OR iFBOT)
| WHAT AND HOW |
|
| FREQUENCY |
|
PROS |
|
CONS |
|
GUAIAC FECAL OCCULT BLOOD TEST (FOBT)
| WHAT AND HOW |
|
| FREQUENCY |
|
PROS |
|
CONS |
|
FLEXIBLE SIGMOIDOSCOPY
| WHAT AND HOW |
|
| FREQUENCY |
|
PROS |
|
CONS |
|
VIRTUAL COLONOSCOPY
| WHAT AND HOW |
|
| FREQUENCY |
|
PROS |
|
CONS |
|
DOUBLE CONTRAST BARIUM ENEMA
| WHAT AND HOW |
|
| FREQUENCY |
|
PROS |
|
CONS |
|
Unfortunately, millions of Americans skip screening and pass on a crucial opportunity to find and treat precancerous conditions or early cancer. It is critical to identify cancer in an early or local stage, before it spreads and becomes more difficult to treat. As mentioned earlier, patients have a 90% five-year survival rate when colorectal cancer is found at an early stage, but that drops significantly — down to just 14% — when cancer is found in an advanced stage and has spread to distant organs.
Colon cancer and rectal cancer affect people of all ages, ethnicities, and lifestyles—no one is immune. Yet we have a powerful defense against this disease: screening. With screening—colorectal cancer is one of the most preventable of all cancers. Make an appointment today to speak to your doctor and see if the time is right for you to proactively minimize your risk of developing colorectal cancer.
Early detection is the key.
